Well...it's been quite a week! I don't know how I managed to make it to work every day. I most certainly didn't cook every day. I didn't have this type of 'all-day-sickness' when I was pregnant with Arianna and I really wasn't prepared.
Today I actually woke up without feeling sick - which was so nice. But I'm drinking lots of sprite zero to help calm my tummy. I also find I have to eat constantly or I get ill. I wish I could ALWAYS pick healthy things to eat, but I don't. It's just before lunch today and so far I've had: Scrambled egg, cheese on a croissant, small pudding cup, granola bar, pear. Lunch will probably be a sm. subway veggie sub with cheese and extra vinegar - I lived on this when pregnant with Arianna and haven't really touched it since. Why does being pregnant make me crave vegetables? I guess it could be worse...
Next Friday is my ultrasound! ahh!!! I'm excited to see the little bean that's been making me SO sick!
Friday, January 25, 2008
Week 7
Posted by Jennifer at 10:55 AM 1 comments
Labels: pregnancy 2
Wednesday, January 23, 2008
I'm still here...
I'm still here, I promise. I'm just so sick with 'all day sickness'. I can't hardly concentrate on anything right now. I hope it only lasts a few weeks and if I'm feeling up to it I'll post more here but right now I just want to curl under a rock and sleep the next 5 weeks away!
Posted by Jennifer at 1:38 PM 0 comments
Labels: pregnancy 2
Friday, January 18, 2008
Week 6
Today I'm half way through my first trimester! ya!!
It's starting to feel more real now. I'm having trouble sleeping as I'm up to the use the bathroom at least once a night. I had my first craving yesterday and boy did it feel great to get it too!
It was a waldorf chicken salad sandwich from a deli near my office. Its chicken with lots of mayo, cranberries, cheddar cheese, lettuce on a wheat wrap. Ahhh... heaven in a sandwich! Today I'm craving a Panera Bread Orchard Harvest salad and can't wait for lunch time!
I also had my first bout with nausea this morning. I was holding Arianna while getting everything ready for work and a wave hit me. I had to put her down and of course, as usual, she screamed and wanted to be picked up again but there was no way I was bending over! Daddy came to the rescue and picked her up though! It's sure going to be tough when I get my cerclage and can't pick her up at all. I hope she doesn't start to favor others just because I can't pick her up.
As I wrote in this post, I've been getting pretty emotional. Yesterday involved breaking down and crying after seeing the NICU Arianna stayed at. I'm determined to all I can in my power to avoid going there again!
Tonight I'm headed to Target to get some maternity jeans and hopefully some regular sweaters - its cold out!
Posted by Jennifer at 8:47 AM 0 comments
Labels: pregnancy 2
Thursday, January 17, 2008
Body fat link to pre-eclampsia
Chemicals in fat tissue may trigger pre-eclampsia in some pregnant women, a study suggests.
Researchers in the United States studied over 1,000 pregnant women. About 6% went on to develop pre-eclampsia.
The condition causes a woman's blood pressure to rise sharply, putting both mother and baby at risk.
The researchers found a direct link between the women's weight before they became pregnant and their risks of developing pre-eclampsia.
Higher risk
For instance, women who were obese before they were pregnant were three times more likely to develop pre-eclampsia compared to those of normal weight.
Women who were overweight were twice as likely to suffer problems. Those who were underweight were half as likely to experience difficulties compared to those of normal weight.
Action on Pre-Eclampsia
In fact, the risks increased steadily depending on how much body fat the women had before they were pregnant.
The researchers, who are based at the Magee Women's Research Institute in Pittsburgh, said this suggested that body fat played a role in determining who was at risk.
While further studies are needed, they suggested that chemicals produced by fat tissue may be responsible.
Speaking at the American Society for Nutritional Sciences annual meeting in Washington, they said the findings could lead to new treatments to protect against the condition.
However, they said the findings also highlighted the importance for women of being normal weight when they become pregnant.
Researchers at the University of Glasgow were recently awarded has almost £129,000 by the British Heart Foundation to carry out work in this area.
They will compare blood plasma from women who have had pre-eclampsia with healthy women.
They believe that in some women plasma can stimulate fat cells and cause them to release excessive amounts of fatty acids and other toxic products triggering pre-eclampsia.
Mike Rich, chief executive of Action on Pre-Eclampsia, said women planning to become pregnant can take action to reduce their risks of developing the condition.
"The Magee research confirms what we have known about increased BMI being linked to a greater risk of pre-eclampsia.
"However, it goes further and shows that even small increases in BMI can be significant.
"There is a clear health message. We would advise all women, pregnant and considering becoming pregnant to eat a sensible and healthy diet in order to help reduce the risk of pregnancy complications such as pre-eclampsia.
"Women should also ensure that they attend all of their antenatal appointments for blood pressure monitoring and urine testing."
Posted by Jennifer at 3:49 PM 0 comments
Labels: Pre eclampsia/HELLP
Pregnancy disorder link to cancer
Women with a history of the pregnancy disorder pre-eclampsia are at greater risk of cancer, research suggests.
The chance of developing breast cancer is "significantly" increased, the study shows.
Research by the Hadassah-Hebrew University in Jerusalem also indicates a greater risk of stomach, ovary, lung and larynx cancer.
A report in the BMJ also suggests environmental and genetic factors may influence pre-eclampsia and cancer.
The study, which found a link to specific cancers, looked at 37,000 women delivering babies in three large hospitals in Jerusalem between 1964 and 1976.
They compared the risk of cancer in those who had experienced pre-eclampsia, with those who had not.
They also looked at the link between social class and other factors including ethnic origin, religion and diabetes on pre-eclampsia - a life-threatening condition which affects about 5-8% of all pregnancies.
It is characterised by a sharp rise in blood pressure and the presence of protein in the urine and occurs in the last three months of pregnancy.
The study revealed that nearly 2,300 women developed cancer for the first time, including 978 (42.6%) of the breast.
'Significant' risk
Pre-eclampsia was recorded in 1,070 women from the study and of these, 40 or 3.7% developed breast cancer.
This compares to 938 or 2.6% of women who got breast cancer among the 36,000 women who did not have pre-eclampsia.
The research team in Israel concluded the risk of breast cancer was "significantly" increased for pre-eclamptic women.
Only a third of the Jerusalem study group originated in Europe - the others were from the Middle East, north Africa, other Western countries and the Americas.
It is believed that in general breast cancer rates are higher among Western women.
The Israeli study also found the risk of cancers of the stomach, ovary, lung and larynx were increased.
The women were followed-up for an average of 29 years.
Genetic link
The study also discovered that West Asian women were more likely to have pre-eclampsia as were those from a lower social class and those with gestational diabetes - the type which occurs during pregnancy.
Dr Simon Vincent of Cancer Research UK said the results of the study were interesting.
"There are likely to be many factors to do with our environment and our health that might increase our risk of developing cancer," he said.
"We already know of some of these factors thanks to research projects, like this one, that look at large numbers of people over a long period of time.
"There are several very large studies, following women over several years, which are currently running in the UK and elsewhere.
"It will be interesting to see if these researchers see the same effects of pre-eclampsia as this study has demonstrated in Israel."
Some, but not all, previous studies have shown a protective effect of pre-eclampsia on breast cancer, although such research has been carried out mainly in northern Europe and North American populations.
The research team suggests there may be a genetic link to both pre-eclampsia and cancer.
They also claim that diet, insulin resistance, smoking or patterns of infection may affect the development of both cancer and pre-eclampsia and their effects may differ between populations.
Posted by Jennifer at 3:38 PM 0 comments
Labels: Pre eclampsia/HELLP
Birth weight pre-eclampsia 'link'
Women who were underweight when they were born are at greater risk of severe pre-eclampsia in pregnancy, a Swedish study involving 6,000 women suggests.
The risk is particularly pronounced if their mothers had pre-eclampsia when pregnant with them, researchers say.
Pre-eclampsia is a common condition which causes high blood pressure and can put the mother's life at risk.
UK experts said doctors should use the findings, reported in BJOG, to identify women who need more careful monitoring.
The researchers looked at more than 6,000 women under the age of 30 years who had been unusually small when they were born and who had given birth themselves.
Women who were underweight when born had a "markedly increased" risk for severe pre-eclampsia during their pregnancy, they said.
If their mothers had also had pre-eclampsia, the risk was doubled.
The research supports previous work suggesting that pre-eclampsia may run in families.
Low birth weight is also believed to be related to other conditions associated with high blood pressure, such as heart disease.
Prevention
Spotting pre-eclampsia early on can be difficult, despite routine monitoring of blood pressure, and knowing who might be more at risk would be useful.
Dr Karin Zetterstrom, study leader and gynaecologist and obstetrician at Orebro University Hospital in Sweden, said pre-eclampsia could be dangerous to a mother and baby in many ways.
"Those who are born underweight also have high risk of heart disease and the severe form of pre-eclampsia might be part of that pathway.
"It might be of value to ask a woman if she was born underweight or if her mother had pre-eclampsia because we know she is at high risk that her pre-eclampsia will turn out to be the severe form."
Professor Andrew Shennan, professor of Obstetrics and Gynaecology at King's College London and spokesperson for the baby charity Tommy's, agreed with the researchers recommendations for identifying and monitoring those at increased risk.
He said finding women at risk of the severe form of the condition was key.
"One of the really important things is distinguishing between early (commonly severe) and late onset pre-eclampsia because early onset is where the problems lie.
"But paradoxically we don't see people very often at that crucial time and that's the time we need increased surveillance."
"This is quite new stuff and a lot of obstetricians may not even be thinking about it," he added.
Professor Phil Steer, BJOG editor-in-chief, said: "What this research demonstrates is the need for careful and detailed history taking when a woman is first seen in pregnancy.
"If we know that the likelihood of a woman developing severe pre-eclampsia is high, increased surveillance during pregnancy and early appropriate management will help to safeguard the health of both mother and baby."
Posted by Jennifer at 3:35 PM 0 comments
Labels: Pre eclampsia/HELLP
Preeclampsia genetic basis
A gene associated with susceptibility to preeclampsia is identified in the May issue of Nature Genetics, explaining why this condition runs in families. Preeclampsia is a common and serious complication of pregnancy, involving elevated blood pressure and impaired kidney function.
Cees Oudejans and colleagues found that the majority of individuals with preeclampsia had received variants of a particular gene from their mother, and suggest that this variant functions less well than most other forms of the gene.
Intriguingly, only the maternal copy of this gene is expressed in the placenta during the critical stage in which it invades the lining of the uterus, explaining why the process is so sensitive to loss of this gene's function.
The loss of appropriate function of this gene in the placenta is suggested as a cause of preeclampsia. The study included 67 cases of preeclampsia amongst families with two or more affected sisters, identified from databases within 22 hospitals in the Netherlands.
Posted by Jennifer at 3:33 PM 0 comments
Labels: Pre eclampsia/HELLP
Take this and shove it!
Emotionalism that is.
Today I had to go to the hospital to get some bloodwork done (non-pregnancy related). The campus that the hospital is at also houses the building for the maternity hospital (different hospitals - confused yet?). The construction around this area is insane.
The hospital I was going to had construction going on - additions to the two largest buildings, one of which spans the street. The maternity hospital has construction going on too. They're building an addition as large as the main hospital. It's just crazy over there. I'm glad I don't have to go there often... yet.
As I rounded the corner to the parking lot I looked close at the construction at the maternity hospital and thought to myself - I hope our next baby doesn't have to see what this new construction looks like (the new building is the new NICU). Then I pulled into the parking lot and parked in a spot I parked in every day for the months Arianna was in the NICU.
Then it hit me.
I could be back here every day at the end of the summer. I could do the NICU ride all over again. I could lose my identity and become a robot going from work to NICU to home to bed and over and over again. I could get to know the cafeteria staff by first names since I'd be eating dinner there every night for moths.
I'm not an emotional person. For anyone that has met me I've fairly level headed (other than the 'short fuse' thing every once in a while *blush*). I pride myself on being pretty composed. I hardly ever cried when Arianna was in the NICU - but I did break down when she went to the PICU just a week after coming home from the NICU.
But today...I cried so hard. I cried for ten minutes. I didn't want to get out of the car and walk to the blood draw station because I knew my face would be all red and puffy. I couldn't find tissues and it made me cry more.
I called my husband and cried to him. All he could understand was "I can't do parking in this lot for months again! I don't want to do the NICU again! I can't, I just can't!"
I hate this emotionalism stuff... pregnancy is for the birds! ;-)
Posted by Jennifer at 2:58 PM 3 comments
Labels: pregnancy 1, pregnancy 2
Does premature birth run in your family?
Premature birth runs in my family - I was born at 30 weeks, my brother at 34 weeks and my daughter at 28 weeks.
There is a study at Washington University School of Medicine that is recruiting people that have a familial history of preterm birth.
If you have a familial history PLEASE sign up for the study.
There are two parts to participating in the F.E.T.A.L. study:
1) Fill out a detailed questionnaire about the births in your family,
especially the premature births. We will mail you this questionnaire
with a self-addressed, stamped envelope for you to return to us at
your convenience to the address you supplied on the web site. We will
also need to send you consent forms that should be filled out for you
and your child stating that you understand the goals, involvement,
risks, and benefits of the research study, which are outlined in the
consent form and will be explained to you by a member of our research
team after you receive it.
2) The second part of the study includes collecting DNA samples from
you and your child (children) to analyze for specific genes which may
be associated with preterm birth. DNA samples can be obtained from a
saliva collection kit which we would mail to you. You can collect the
saliva samples of members of your family who wish to participate, and
then mail them back to us at the Center for Preterm Birth Research.
Regardless of whether or not you choose to provide DNA samples, we
would appreciate your participation by completing the questionnaire.
The information provided in this form will provide us with valuable
information pertinent to our study.
Please click here to learn more.
I hope you can all agree that it would give all preemie moms great joy to know they helped further the study of why preterm birth occurs and possibly find a cure!
Posted by Jennifer at 10:23 AM 2 comments
Labels: Premature Birth
Wednesday, January 16, 2008
Feeling happy?
Any mom who is in a high risk pregnancy can probably relate to this post.
I'm pregnant again - I should be happy and making plans, choosing names, buying clothes etc. But I'm not.
Instead I'm investigating ways to get to the illustrious 40 week point. I'm investigating cerclage and infection rates. Instead of telling family and friends I'm hoping to make it to my next appointment to get the 'plan of action'.
I feel like I can't get excited and happy. I feel like any excitement I may have will get ripped from my heart in one fell swoop... so why set myself up for that? Why get excited when you could possibly have the worst possible outcome?
I knew, going into this pregnancy, that there would be nothing 'normal' about it. But I didn't really think about the stress that would go with it too much. Like my work - what if they don't let me work from home while on bed rest? Who will care for my daughter if I'm on bed rest? Can we afford to keep the nanny that watches her if my work won't let me work from home? How will I get to doctors appointments? Will my husband totally resent not having sex after I reach 15 weeks and get my cerclage? Will our relationship be stressed beyond repair? How will I keep my sanity laying in bed 24/7?
I hope for the best, but prepare for the worst. I wish it didn't have to be that way.
Posted by Jennifer at 1:25 PM 2 comments
Labels: pregnancy 2
Monday, January 14, 2008
Today I'm 5 weeks 3 days...
...and I had to break out the maternity pants. I can't 'suck it in' anymore.
I can't believe this!! SERIOUSLY. I didn't wear maternity jeans with Arianna until I was nearly 20 weeks and went into labor when I was at the store buying my first maternity outfit - this is just unreal to me.
I'm actually a little nervous so I hope some moms of 2 or more can put my mind at ease.
Were you showing this early with your second (or third etc.) or do I have to be worried about multiples?
UPDATE: Ok, took a few days but the 'bloat' is gone. Back into regular clothes! ha!
Posted by Jennifer at 9:13 PM 8 comments
Labels: pregnancy 2
Sunday, January 13, 2008
Women Successfully Treated to Prevent Preterm Labor at Low Risk for Recurrent Episode
ROCHESTER, Minn. — Mayo Clinic and Medical University of South Carolina researchers have found that the large majority of expectant mothers treated to prevent preterm labor will deliver at or near term.
"We found that if you stopped labor once, only one out of nine women would come back with a repeat episode, which is about a baseline risk for preterm delivery," says Brian Brost, M.D., Mayo Clinic high-risk pregnancy specialist and study co-author. "Most babies will do just fine — they are delivered near term or at term."
While expectant mothers treated with magnesium for preterm labor commonly feel queasy or flushed, serious side effects are rare, according to Dr. Brost, and they usually result from improper dosage or monitoring of the patient following treatment.
The investigators also studied whether the expectant mothers whose preterm labor did recur would be candidates for a steroid treatment in addition to the magnesium. The goal of steroid treatment is to promote accelerated development of the baby's lungs and other body systems. In order for the steroid to be delivered and absorbed into the baby's system, the repeat magnesium treatment to inhibit uterine contractions would need to delay labor for at least 24 to 48 hours. In this study, the researchers found that the magnesium could delay labor long enough for the steroid to work in about half the cases.
This study was conducted retrospectively by analyzing delivery records for consecutive preterm labor patients at Mayo Clinic. In 154 expectant mothers treated for preterm labor who were still undelivered one week later, 87.7 percent (135 women) delivered their babies at greater than 34 weeks. After 34 weeks, standard procedure is to deliver the baby rather than treat the mother again if she went into labor, according to the study's researchers.
In 19 women, or 12.3 percent, preterm labor recurred. Repeat magnesium treatment to inhibit uterine contractions delayed labor for at least 24 to 48 hours in 11 women, offering the possibility for steroid therapy. The other eight women with repeat preterm labor delivered within 24 hours of readmission to the hospital, which did not allow enough time for the physicians to consider giving the steroid treatment.
No measures have been shown to definitively prevent preterm labor, according to Dr. Brost. At the same time, he says, rates of preterm labor have been slowly but steadily rising in the last several decades in the United States.
Newborns are considered to be full-term when delivered about 40 weeks after the first day of their mother's last menstrual period.
To obtain the latest news releases from Mayo Clinic, go to www.mayoclinic.org/news. MayoClinic.com (www.mayoclinic.com) is available as a resource for your health stories.
Posted by Jennifer at 12:22 PM 2 comments
Labels: Preterm Labor
Magnesium Sulfate More Effective Than Nifedipine in Preventing Preterm Delivery
June 29, 2007 — Magnesium sulfate is more effective than nifedipine in preventing preterm delivery for 48 hours, but nifedipine is linked with fewer maternal adverse events, according to the results of a randomized controlled trial published in the July issue of Obstetrics & Gynecology.
"Magnesium sulfate is the most commonly used first-line tocolytic in North America although it has not been demonstrated to be superior to saline infusion, and its use has been a source of controversy," write Deirdre J. Lyell, MD, from Stanford University Medical Center and Lucile S. Packard Children's Hospital in California, and colleagues. "Magnesium sulfate requires intravenous administration, has potential for overmedication with serious maternal adverse effects and may be associated with adverse neonatal effects.... Nifedipine may be more easily tolerated, is administered orally, and appears to have few adverse effects."
The objective of this multicenter randomized study was to compare the efficacy and adverse effects of intravenous magnesium with those of oral nifedipine for acute tocolysis of preterm labor in 192 patients in active preterm labor who were at 24 to 33 weeks and 6 days of gestation. The main endpoint was arrest of preterm labor, defined as prevention of delivery for 48 hours with uterine quiescence.
Compared with women treated with nifedipine, more women treated with magnesium sulfate achieved the main endpoint (87% vs 72%; P = .01). Both groups were similar in delivery within 48 hours (7.6% magnesium sulfate vs 8.0% nifedipine; P = .92), gestational age at delivery (35.8 vs 36.0 weeks; P = .61), birth before 37 and 32 weeks (57% vs 57%; P = .97 and 11% vs 8%; P = .39, respectively), and episodes of recurrent preterm labor.
In the magnesium sulfate group, mild and severe maternal adverse effects were significantly more frequent than in the nifedipine group. Although average birth weight, birth weight less than 2500 g, and neonatal morbidities were similar in both groups, newborns of mothers in the magnesium sulfate group spent longer in the neonatal intensive care unit (8.8 ± 17.7 vs 4.2 ± 8.2 days; P = .007).
Study limitations include lack of double-blinding or placebo control and failure to establish the optimal doses of magnesium sulfate and nifedipine.
"Patients who received magnesium sulfate achieved the primary outcome more frequently," the authors write. "However, delay of delivery, gestational age at delivery, and neonatal outcomes were similar between groups. Nifedipine was associated with fewer maternal adverse effects."
The Division of Maternal–Fetal Medicine at Stanford University and the Department of Obstetrics and Gynecology at Santa Clara Valley Medical Center supported this study. The authors have disclosed no relevant financial relationships.
Obstet Gynecol. 2007;110:61-67.
Posted by Jennifer at 12:18 PM 0 comments
Labels: Preterm Labor
Saturday, January 12, 2008
Vitamin C supplementation to prevent premature rupture of the chorioamniotic membranes: a randomized trial
Esther Casanueva, Carmina Ripoll, Maricruz Tolentino, Rosa Maria Morales, Frania Pfeffer, Pablo Vilchis and Felipe Vadillo-Ortega
1 From the Public Health Research Branch (EC, CR, MT, RMM, and FP), the Department of Obstetrics and Gynecology (PV), and the Direction of Research (FV-O), National Institute of Perinatology, Mexico City, Mexico.
Background: Vitamin C is involved in the synthesis and degradation of collagen and is important for maintenance of the chorioamniotic membranes. Inadequate availability of ascorbic acid during pregnancy has been proposed as a risk factor for premature rupture of the chorioamniotic membranes (PROM).
Objective: The objective of the study was to evaluate the effectiveness of 100 mg vitamin C/d in preventing PROM.
Design: A controlled double-blind trial was performed. Pregnant women (n = 126) in their 20th wk of gestation were invited; 120 accepted and were randomly assigned to 2 groups (100 mg vitamin C/d or placebo). Every 4 wk, plasma and leukocyte vitamin C concentrations were measured, and each subject was evaluated for cervicovaginal infection. The incidence of PROM was recorded for each group as an indicator of the protective effect of vitamin C supplementation.
Results: One hundred nine patients finished the study. Mean plasma vitamin C concentrations decreased significantly throughout the pregnancy in both groups (P = 0.001), and there were no significant differences between groups. Between weeks 20 and 36, mean leukocyte vitamin C concentrations decreased from 17.5 to 15.23 µg/108 cells in the placebo group and increased from 17.26 to 22.17 µg/108 cells in the supplemented group (within- and between-group differences: P = 0.001). The incidence of PROM was 14 per 57 pregnancies (24.5%) in the placebo group and 4 per 52 pregnancies (7.69%) in the supplemented group (relative risk: 0.26; 95% CI: 0.078, 0.837).
Conclusion: Daily supplementation with 100 mg vitamin C after 20 wk of gestation effectively lessens the incidence of PROM.
Posted by Jennifer at 8:43 PM 4 comments
Labels: pPROM
Vitamins C and E in the latency period in women with preterm premature rupture of membranes
S. Bornaa, Corresponding Author Contact Information, H. Bornab and B. Daneshbodie
aDepartment of Perinatology, Tehran University of Medical Sciences, Tehran, Iran
bDepartment of Pediatrics, Shahed University of Medical Sciences, Tehran, Iran
Received 1 December 2004; accepted 23 March 2005. Available online 23 May 2005.
Abstract
Objective: To determine whether supplementation with vitamins C and E after preterm premature rupture of membranes (PPROM) is associated with an increased latency period. Methods: In this double-blind, randomized, controlled trial, 60 women with singleton pregnancies of 26 to 34 weeks' duration and PPROM were randomly assigned to vitamin C (500 mg/day) and vitamin E (400 IU/day) or placebo until delivery. All women received 2 doses of betamethasone in the first 24 h after admission as well as broad-spectrum antibiotic prophylaxis.
Results: Important demographic, as well as clinical characteristics such as number of cases of chorioamnionitis, early neonatal sepsis, and respiratory distress syndrome, were similar in the 2 groups. A statically significant difference in the mean ± S.D. number of days of latency was found between the groups (10.5 ± 5.2 days vs. 3.5 ± 4.0 days (P = 0.03).
Conclusion: Vitamins C and E supplementation of after PPROM is associated with a longer latency before delivery.
Posted by Jennifer at 8:34 PM 0 comments
Labels: pPROM
Friday, January 11, 2008
Carbon Monoxide May Help Prevent Debilitating Pregnancy Condition
New findings by Queen's University researchers suggest that administering low doses of carbon monoxide to pregnant women may help prevent the potentially damaging effects to mother and baby of pre-eclampsia.
The study was precipitated by the fact that mothers who smoke cigarettes during pregnancy have a 33 per cent decreased risk of developing pre-eclampsia compared to nonsmokers.
A debilitating condition that affects five to seven per cent of pregnancies, pre-eclampsia is characterized by high blood pressure in pregnant women and is one of the leading causes of baby and maternal deaths. "At present there is no cure or effective treatment for this condition, other than delivery of the baby," says research team leader Dr.Graeme Smith (Obstetrics and Gynecology), an expert in high-risk obstetrics.
In the Queen's study, published in the September issue of the American Journal of Pathology, tissue from the placentas of nonsmoking women who had delivered babies by caesarian section was exposed to the same kind of oxidative stress -- not enough oxygen being supplied through the blood -- experienced by women with pre-eclampsia. When the tissues were treated with carbon monoxide, at levels similar to those found in the blood of smoking mothers, cell death in the placenta was significantly reduced.
"We believe that carbon monoxide found in cigarette smoke, and subsequently carried in a smoking mother's blood, may be the cause of their lower risk of developing pre-eclampsia," says Dr. Smith. He stresses however that any perceived benefit of smoking during pregnancy is outweighed by the many risks: premature membrane rupture, preterm delivery, stillbirth, low birth weight, and sudden infant death syndrome.
Produced naturally by the body at low levels, carbon monoxide relaxes blood vessels and may prevent the death of placental cells, which can cause injury to fetus and mother. Future studies will determine whether carbon monoxide can prevent placental cell death in animal models and whether other approaches similar to carbon monoxide may provide protection.
Also on the research team, from Queen's Department of Anatomy and Cell Biology, are: Shannon Bainbridge, Louiza Belkacemi, Michelle Dickinson, and Charles Graham.
The work was supported by the Strategic Training Initiative in Research in Reproductive Health Sciences, the Heart and Stroke Foundation of Ontario, and the Canadian Institutes of Health Research.
Adapted from materials provided by Queen's University.
Posted by Jennifer at 3:59 PM 0 comments
Labels: Pre eclampsia/HELLP
Old Drug Being Tested As Possible Pre-eclampsia Cure
Researchers at the University of Texas Medical Branch at Galveston are trying to determine whether a drug already available to heart patients can also be used to delay delivery in expectant mothers with severe preeclampsia. If so, this groundbreaking study would give hope to hundreds of thousands of women who experience this life-threatening disorder each year.
The drug, Digibind, has been prescribed for over 20 years to patients who overdose on a certain heart medication, but is not yet approved for preeclampsia, the most common and dangerous pregnancy complication affecting as many as eight in every 100 pregnant women. The disorder is characterized by high blood pressure, protein in the urine and multi-organ dysfunction, all of which can seriously harm both mother and fetus.
"Preeclampsia is the No. 1 killer of pregnant women in the world, and there is no cure except delivery," said Dr. George Saade, chief of maternal--fetal medicine at UTMB. "When it is severe and occurs early in the pregnancy, delivery in order to protect the mother results in a premature baby. That's why this study is important, because if the medication works, then we can protect the mom while allowing the baby to grow and develop without delivering early."
The clinical trial will test whether Digibind reverses or prevents the abnormalities that occur with preeclampsia and allows the fetus to remain in the womb longer. This would give doctors more time to administer steroids to prevent respiratory complications in premature births and reduce the need for costly and lengthy neonatal intensive care.
"Right now, there is no treatment for preeclampsia, so this is truly groundbreaking," said Dr. Nicole Ruddock, the study's principal investigator and an instructor in UTMB's Department of Obstetrics and Gynecology.
UTMB will continue enrolling participants at least through the end of this year. The study is sponsored by Protherics and is taking place in eight states around the country.
Adapted from materials provided by University of Texas Medical Branch at Galveston.
Posted by Jennifer at 3:54 PM 0 comments
Labels: Pre eclampsia/HELLP
Lack Of Well-Being In A Pregnant Woman May Lead To Premature Delivery
A group of researchers of the University of Modena has investigated the role of psychological well-being in premature delivery. The study is reported in a recent issue of Psychotherapy and Psychosomatics.
The aim of this study was to evaluate how sociodemographic factors, psychosocial adaptation to pregnancy and well-being levels are associated with the onset of preterm uterine contractions allowing symptomatic preterm labor. In a prospective case-control design, 51 consecutive women admitted for threatened preterm labor were enrolled.
The patients received standard care. The day before discharge, once contractions had been stopped, the patients were administered 2 questionnaires: the Prenatal Self-Evaluation Questionnaire of Lederman and the Psychological Well-Being Scales. Controls were enrolled among asymptomatic, healthy women attending routine prenatal care.
They were matched for parity and gestational age. Gestational age at inclusion ranged from 25 to 34 weeks. Fourteen cases and 4 controls delivered preterm. Cases were less educated than controls, showed a lower acceptance of pregnancy and worse relationship with others, namely with the husband, compared to controls.
They also displayed a reduced environmental mastery. Having a low education, poor relationship with others, including the husband, and impaired coping skills appeared to be independent risk factors for the development of symptomatic preterm labor in urbanized women.
Journal reference: Facchinetti, F. ; Ottolini, F. ; Fazzio, M. ; Rigatelli, M. ; Volpe, A. Psychosocial Factors Associated with Preterm Uterine Contractions. Psychother Psychosom 2007;76:391-394
Ya know what's a bit scary about this? Any woman who is pregnant after a preemie is going to be a NERVOUS wreck (I have yet to talk with one who isn't). Where does that put us according to this study? Even more at risk for preterm birth... ugh!
Posted by Jennifer at 3:52 PM 0 comments
Labels: Premature Birth
Home Uterine Monitors Not Useful For Predicting Premature Birth
Portable monitors that detect contractions of the uterus do not appear to be useful for identifying women likely to have a preterm delivery, according to a study by the National Institute of Child Health and Human Development (NICHD).
Although they are widely prescribed for women at risk of giving birth prematurely, the NICHD study confirms earlier findings that the monitors are not useful for predicting or preventing preterm birth. The study also confirmed that several other methods being assessed as ways to predict preterm labor were of little value.
"The study found that while women who gave birth prematurely did have slightly more contractions throughout pregnancy than did women who gave birth at term, there was no detectable pattern that would predict premature birth," said Duane Alexander, M.D., Director of the NICHD.
The study was conducted at the 11 centers participating in the NICHD Network of Maternal-Fetal Medicine Units and appears in the January 25 New England Journal of Medicine. The study was led by Jay Iams, M.D., director of the Division of Maternal-Fetal Medicine at the Ohio State University Medical Center.
The portable, or ambulatory, monitors cost up to $100 a day and may be worn for up to 10 weeks. The monitors relay information to a central monitoring office, where any potential signs of early labor can be passed on to a physician.
The researchers analyzed 34,908 hours of recordings from 306 women. When the women began the study, they were in their 22nd through 24th week of pregnancy. The authors wrote that the women who gave birth before the 35th week of pregnancy had a slightly greater frequency of contractions than did the women who gave birth after the 35th week, but this information did not allow them to predict impending premature labor. A pregnancy is considered full term at 37 weeks.
"…we could identify no threshold frequency that effectively identified women who delivered preterm infants," the study authors wrote in the New England Journal of Medicine article.
The researchers also found little value of some other techniques in predicting preterm labor, including measuring the cervix and collecting a substance known as fetal fibronectin from the cervix.
"Our data indicate that ambulatory monitoring of uterine contractions does not identify women destined to have preterm delivery," the authors wrote.
Preterm birth complicates from 8 to 10 percent of all births, said Catherine Spong, M.D., Chief of NICHD's Pregnancy and Perinatology Branch and coordinator of the Maternal-Fetal Medicine Units. Premature infants are at greater risk for life-threatening infections, for a serious lung condition known as respiratory distress syndrome, and for serious damage to the intestines (necrotizing enterocolitis). Most deaths of premature infants occur among those born before the 32nd week of pregnancy. In addition, the cost of caring for premature infants in the United States exceeds $4 billion each year.
Posted by Jennifer at 3:50 PM 0 comments
Labels: Premature Birth, Preterm Labor
3-D Ultrasound Identifies Women At Risk For Impending Preterm Birth
To help physicians non-invasively identify women at risk for preterm birth, 3-D ultrasound was used to measure the size of fetal adrenal glands, according to an abstract presented by Yale School of Medicine researchers at the Society for Maternal-Fetal Medicine Conference February 8, 2007 in San Francisco.
Preterm birth is a major public health problem with lasting repercussions on families and society. The authors found that the ultrasound measurements could identify a preterm risk of delivery within five days of the measurement.
"Our results suggest that examining the fetal adrenal gland at the time a woman is evaluated for symptoms of preterm labor, may have major beneficial clinical implications," said first author Ozhan Turan, postdoctoral fellow in the Department of Obstetrics, Gynecology & Reproductive Sciences at Yale School of Medicine. Turan conducted the study with senior author Catalin Buhimschi, M.D., director of Perinatal Research at Yale Ob/Gyn.
The authors said that understanding the time when a marker becomes positive in relationship to preterm birth is essential for a test with high diagnostic accuracy. "The high accuracy, sensitivity and specificity of the adrenal gland volume in predicting preterm birth within five days from the time of examination proves that 3-dimensional ultrasound evaluation of the fetal adrenal gland has the desired test characteristics to define a population at risk," they said.
The current study creates the basis for further prospective studies to confirm that 3-dimensional ultrasound assessment of the fetal adrenal gland volume can assist clinicians with devising better therapeutic and preventive interventions for preterm birth.
Other authors on the abstract included Sifa Turan, Edmund Funai, Irina Buhimschi and Joshua Copel.
Abstract Title: "Three-dimensional (3D) Ultrasound Measurement of Fetal Adrenal Gland Volume. A Novel Method of Identifying the Patient at Risk for Impending Preterm Birth."
Adapted from materials provided by Yale University.
Posted by Jennifer at 3:47 PM 0 comments
Labels: Premature Birth
In Hispanic Women, Genetic Variations Linked To Spontaneous Preterm Birth
Preterm birth is a major cause of illness and death in newborns. A genetic cause of preterm birth was suggested by racial disparity, a tendency to occur within families and a high rate of recurrence, according to Errol Norwitz, M.D., associate professor in the Department of Obstetrics, Gynecology & Reproductive Sciences at Yale and lead investigator of the study.
Norwitz and his team prepared DNA samples from 102 mothers with a spontaneous unexplained preterm birth and 408 mothers who delivered at term with no complications. They then compared the distribution of 128 well-known genetic variations, known as single nucleotide polymorphisms, in 77 genes between the two groups. The patients in the study were identified from the March of Dimes Perinatal Epidemiology Research Initiative Project at Yale and New York University between January 1989 and June 2005.
"Our analysis demonstrates that, in an Hispanic population, mothers who carried any one of four polymorphisms were significantly more likely to have a spontaneous preterm birth," said Norwitz.
The four polymorphisms included CYP2C9S144, IL6S174, CCR5S1 and ENPP1S121. The risk of preterm birth was highest among women with the ENPP1 variant.
"The strong association of ENPP1 was particularly compelling, but how this variant functions and why it predisposes preterm births still needs to be determined," said Norwitz.
In another abstract using the same study subjects, Norwitz and colleagues explored whether polymorphisms in the gene that encodes the progesterone receptor may identify women at risk for preterm birth. The team found no such association.
"Progesterone supplementation may prevent preterm birth in about 30 to 40 percent of women at high risk by virtue of a prior preterm birth, but exactly how progesterone supplementation works is still unknown," said Norwitz. "While this was a negative finding, it was an important question to answer."
Other authors on both abstracts included Thomas Morgan, Victoria Snegovskikh, Edward Kuczynski, Hee Joong Lee, Frederick Schatz, Se-Te Joseph Huang, Catalin Buhimschi, Edmund Funai, Irina Buhimschi, Antonette Dulay, Guoyang Luo, Sonya Abdel-Razeq and Charles Lockwood.
Abstract #297: "Identification of Single Nucleotide Polymorphisms in Maternal Genes Associated with Spontaneous Preterm Birth."
Abstract # 316: "Single Nucleotide Polymorphisms in the Human Progesterone Receptor (PR) Gene and Spontaneous Preterm Birth."
Adapted from materials provided by Yale University.
Posted by Jennifer at 3:46 PM 0 comments
Labels: Premature Birth
Progesterone Injections Do Not Prevent Preterm Birth In Twin Pregnancies, Study Finds
The result came as a surprise to the researchers, who previously discovered that weekly injections of the naturally occurring hormone, called 17 alpha-hydroxyprogesterone or 17-OHPC, reduced additional preterm births by one-third in women whose previous babies were born prematurely.
"Based on the results of the first study, which showed that 17-OHPC reduced preterm birth in the group with the highest risk, we were hopeful that it would also prevent preterm birth in twin pregnancies, which represents an intermediate level of risk," said John Thorp, M.D., a study co-author and professor of obstetrics and gynecology UNC-Chapel Hill. "The mechanisms that lead to preterm birth are complex, and I think our current study shows they may not be amenable to a single solution."
The study results are published in the Aug. 2 issue of The New England Journal of Medicine. The lead author is Dwight J. Rouse, M.D., of the University of Alabama at Birmingham. The study was conducted for the Maternal-Fetal Medicine Units Network of the National Institute of Child Health and Human Development, which provided grant funding. It took place at 14 sites across the United States, including UNC-Chapel Hill, WakeMed and the Wake County Health Department.
For the study, 655 healthy women with twin pregnancies and no prior preterm births received weekly injections of either 17-OHPC or placebo, starting at 16 to 20 weeks into their pregnancies and ending at 35 weeks. The results showed no meaningful difference between the 17-OHPC and placebo groups. Birth or miscarriage before 35 weeks gestation occurred in 41.5 percent of the 17-OHPC group and in 37.3 percent of the placebo group.
The researchers concluded that treatment with 17-OHPC did not reduce the rate of preterm birth in women with twins.
"Why 17-OHPC is effective in reducing the rate of preterm birth in women with a prior spontaneous preterm birth, but not in women carrying twins is a question that will be answered only when the mechanisms underlying preterm birth and the actions of 17-OHPC are better understood," they wrote, adding that additional research is needed to see whether 17-OHPC is effective in other conditions in which the risk of preterm birth is increased.
Thorp said the same research network is currently working on two other 17-OHPC studies. One involves women with triplets while the other focuses on women with a short cervix. Both groups are considered to have an intermediate risk of preterm birth.
Another question for future research, Thorp said, is whether or not injections are the best method for administering 17-OHPC. It's worth investigating whether other methods, such as daily vaginal suppositories, might be more effective, he said.
A commercial formulation of the drug, marketed under the name Gestiva, has been granted orphan drug status by the Food and Drug Administration and an application for full FDA approval is pending.
Posted by Jennifer at 3:43 PM 1 comments
Labels: Multiples, Premature Birth, Preterm Labor
Metronidazole to Prevent Preterm Delivery in Pregnant Women with Asymptomatic Bacterial Vaginosis
Background Bacterial vaginosis has been associated with preterm birth. In clinical trials, the treatment of bacterial vaginosis in pregnant women who previously had a preterm delivery reduced the risk of recurrence.
Methods To determine whether treating women in a general obstetrical population who have asymptomatic bacterial vaginosis (as diagnosed on the basis of vaginal Gram's staining and pH) prevents preterm delivery, we randomly assigned 1953 women who were 16 to less than 24 weeks pregnant to receive two 2-g doses of metronidazole or placebo. The diagnostic studies were repeated and a second treatment was administered to all the women at 24 to less than 30 weeks' gestation. The primary outcome was the rate of delivery before 37 weeks' gestation.
Results Bacterial vaginosis resolved in 657 of 845 women who had follow-up Gram's staining in the metronidazole group (77.8 percent) and 321 of 859 women in the placebo group (37.4 percent). Data on the time and characteristics of delivery were available for 953 women in the metronidazole group and 966 in the placebo group. Preterm delivery occurred in 116 women in the metronidazole group (12.2 percent) and 121 women in the placebo group (12.5 percent) (relative risk, 1.0; 95 percent confidence interval, 0.8 to 1.2). Treatment did not prevent preterm deliveries that resulted from spontaneous labor (5.1 percent in the metronidazole group vs. 5.7 percent in the placebo group) or spontaneous rupture of the membranes (4.2 percent vs. 3.7 percent), nor did it prevent delivery before 32 weeks (2.3 percent vs. 2.7 percent). Treatment with metronidazole did not reduce the occurrence of preterm labor, intraamniotic or postpartum infections, neonatal sepsis, or admission of the infant to the neonatal intensive care unit.
Conclusions The treatment of asymptomatic bacterial vaginosis in pregnant women does not reduce the occurrence of preterm delivery or other adverse perinatal outcomes.
Posted by Jennifer at 3:40 PM 0 comments
Labels: Premature Birth, Preterm Labor
Terbutaline: Can it prevent preterm labor?
There is no evidence that beta-mimetic drugs, such as terbutaline and ritodrine, prevent preterm birth. However, beta-mimetics are effective in temporarily reducing or stopping contractions in women who are having preterm labor.
Beta-mimetics are best used to delay delivery long enough — usually 24 to 48 hours — to allow treatment with corticosteroids to speed fetal lung development. Beyond that use, it isn't clear that the benefits of beta-mimetics outweigh the potential risks for the mother. Adverse effects from beta-mimetic drugs may include fluid in the lungs (pulmonary edema) and abnormal heart rhythms (arrhythmias).
Posted by Jennifer at 3:37 PM 0 comments
Labels: Preterm Labor
Relaxation Techniques during pregnancy
Relaxing during pregnancy is important. Research has shown that stress can increase the likelihood that you will have a premature birth. Personally I try to have some amount of time during the day that is dedicated to stress relief. This is something I did not do in my first pregnancy.
Pregnancy can be a stressful time. Your body is going through major changes you’re supporting a tiny growing baby inside you and you’re thwarted by all sorts of pregnancy side-effects, like morning sickness and aching legs. If you’re trying to cope with working, looking after the rest of your family and keeping up with your usual routine, it can all get too much at times.
But it’s important to take time out for yourself and relax and both you and your baby will benefit. Research shows that if you’re regularly stressed, anxious and tense during your pregnancy, you’ve got a greater chance of having a baby that also suffers from stress and anxiety. So if you need some inspiration as to how to relax, here are some helpful tips!
1. Put your feet up. Aching legs and ankles are a common problem in pregnancy, especially in the third trimester, so give yourself regular breaks and take the pressure of your feet. Sit in a comfy chair with your feet on a footstool or propped up on cushions, lie on the sofa or lie on your bed – whatever is comfortable for you. If your ankles are swelling, stack several cushions together to raise your feet up higher, as this helps reduce swelling.
2. Listen to calming music. Take time out from the madness of life and whisk yourself away to a calmer place, with the help of some relaxing music. Choose one of your favourites or treat yourself to a special pregnancy relaxation CD. Sit back, close your eyes and let the music wash over and relax you.
3. Have a massage. Massage is great for easing tension and relaxing the muscles. Rope your partner in to give you a massage or book a treatment with a specialist (many places offer special treatments for pregnant women).
4. Try a reflexology treatment. Reflexology is a natural therapy that believes your feet are in a sense a ‘map of your body.’ A reflexologist will clear blockages and ease ailments by putting a small amount of pressure on your feet – it’s a bit like a foot massage. It can be very relaxing, can relieve tension and help any pregnancy ailments you’re suffering from. (but get someone who is trained in this and has pregnancy experience as some reflexology can actual start labor in a more advanced pregnancy)
5. Have a go at antenatal yoga. Yoga designed for pregnancy can help tone up your body, but most classes also teach special relaxation tips too. These can help relieve any stress you’re experiencing during pregnancy, as well as ease worry about the birth itself. Ask you midwife for antenatal yoga class recommendations.
6. Try meditation or visualisation. Relaxing your mind is just as important as relaxing your body, but it can be hard to do. Meditation or visualisation could help and there are lots of CDs and classes available that teach it especially with pregnancy in mind.
7. Have a laugh. Laughter is a great form of natural – and free – therapy. Meet up with your friends, or watch your favourite comedy or film and have a good laugh. Your baby will pick up on the feel-good factor too.
8. Get some fresh air and sunshine. It’s good to get fresh air and sunshine when you can and can be a good pick-me-up if you’ve been inside all day. Have a stroll around your neighbourhood, walk to the park or even walk around the shops, breathe in the fresh air and relax.
9. Enjoy a night out with your partner. Spend some time unwinding and relaxing together – especially if it’s your first baby, as life will change when it arrives. Have a lovely meal, go to the theatre or indulge in your favourite pastime.
10. Enjoy water. Water is another form of natural healer. Swimming is ideal during pregnancy, as the water is supportive, and it’s not too exhausting. If you fancy a class, most places offer antenatal swimming sessions, but if a swimming pool isn’t your cup of tea, enjoy a nice long soak in the bath instead.
And finally, enjoy the course of your pregnancy. The nine months will fly by and a new baby will soon be part of your life.
Posted by Jennifer at 1:48 PM 0 comments
Labels: General Pregnancy, Premature Birth
Cervical Cerclage
When a woman’s cervix is weak (sometimes called an incompetent cervix) she is more likely to have a baby born prematurely because the cervix shortens or opens too early. In order to prevent premature labor, a woman’s doctor may recommend a cervical cerclage. A cerclage is used to prevent these early changes in a woman’s cervix, thus preventing premature labor. A closed cervix helps a developing baby stay inside the uterus until the mother reaches 37-38 weeks of pregnancy.
What is cervical cerclage?
Treatment for cervical incompetence is a surgical procedure called cervical cerclage, in which the cervix is sewn closed during pregnancy. The cervix is the lowest part of the uterus and extends into the vagina.
Why is cervical cerclage used?
A cervical cerclage procedure may be used if a woman’s cervix is at risk of opening under the pressure of the growing pregnancy. A weak cervix may be the result of:
- History of second-trimester micarriages
- A previous “cone biospy” or a “LEEP” procedure
- Damaged cervix by pregnancy termination
When is a cervical cerclage used?
The best time for the cervical cerclage procedure is in the third month (12-14 weeks) of pregnancy. However, some women may need a cerclage placed later in pregnancy; this is known as an emergent cerclage and is necessary after changes such as opening or shortening of the cervix have already begun. If an emergent cerclage is required, future pregnancies will probably also require a cervical cerclage.
What are alternatives to the cervical cerclage procedure?
If changes in the cervix are found very late in pregnancy, or if the cervix has already opened up significantly, bed rest may be the best alternative.
What are the benefits of a cerclage?
Cervical cerclage helps prevent miscarriage or premature labor caused by cervical incompetence. The procedure is successful in 85% to 90% of cases. Cervical cerclage appears to be effective when true cervical incompetence exists, but unfortunately the diagnosis of cervical incompetence is very difficult and can be inaccurate.
Why doesn’t every woman who has had a preterm baby need a cerclage?
Only women with an abnormal or “incompetent” cervix can be helped by a cerclage. However, even with the help of a cerclage, other problems can cause labor to begin too early. Women who have a cerclage placed will need to be checked routinely for other complications such as infection and preterm labor.
What should I expect before my cervical cerclage is placed?
- Your medical history will be reviewed
- A thorough exam of your cervix including a transvaginal ultrasound performed by a doctor who specializes in high risk pregnancies
- Your doctor will discuss pain control options for the procedure
- Write down any questions or concerns you may want to discuss with your health care provider
What happens during the cervical cerclage procedure?
Most women have general, spinal, or epidural anesthesia for pain control during the procedure. A doctor will stitch a band of strong thread around the cervix, and the thread will be tightened to hold the cervix firmly closed.
What can I expect after the procedure?
- You may stay in the hospital for a few hours or overnight to be monitored for premature contractions or labor.
- Immediately after the procedure you may experience light bleeding and mild cramping, which should stop after a few days. This may be followed by an increased thick vaginal discharge, which may continue for the remainder of the pregnancy.
- You may receive medication to prevent infection or preterm labor.
- For 2-3 days after the procedure, plan to relax at home; avoid any unnecessary physical activity.
- Your doctor will discuss with you when would be the appropriate time to resume regular activites.
- Abstinence from sexual intercourse is often recommended for one week before and at least one week after the procedure.
How long is the cerclage stitch left in?
Generally the thread is removed at the 37th week of pregnancy, but it can be removed before if a woman’s water breaks or contractions start. Most stitches are removed in the doctor’s office without any problems. The procedure is similar to having a pap smear and may cause some light bleeding.
What are the risks of having a cerclage placed?
The likelihood of risks occuring is very minimal, and most health professionals feel a cerclage is a life saving procedure that outweighs the possible risks involved. Possible risks could include:Are there signs I should look for after the cerclage is placed that indicate a problem?
- Premature contractions
- Cervical dystocia (inability of the cervix to dilate normally in the course of labor)
- Rupture of membranes
- Cervical infection
- Cervical laceration if labor happens before the cerclage is removed
- Some risks associated with general anesthesia include vomiting and nausea
It is important to contact your doctor if you experience any of the following symptoms after your cerclage is placed:What about future pregnancies?
- Contractions or cramping
- Lower abdominal or back pain that comes and goes like labor pain
- Vaginal bleeding
- A fever over 100 F or 37.8 C, or chills
- Nausea and vomiting
- Foul-smelling vaginal discharge
- Your water breaking or leaking
Most women who need a cerclage in one pregnancy will need to have a cerclage placed in future pregnancies.
Posted by Jennifer at 12:45 PM 0 comments
Labels: Incompetant Cervix
Dizziness in Pregnancy
Dizziness or feeling faint is a normal symptom during pregnancy. It is more common in the first trimester, but it may also be prevalent throughout your pregnancy.
What causes dizziness during pregnancy?
The main cause of dizziness in pregnancy is due to the rising hormones that cause your blood vessels to relax and widen. This helps increase the blood flow to your baby, but it slows the return of the blood in the veins to you. This causes your blood pressure to be lower than usual, which can reduce the blood flow to your brain, temporarily causing dizziness.
Dizziness is also caused by low blood sugar levels that may occur as your body adapts to changes in your metabolism. Women who are anemic or who have varicose veins may be more susceptible to dizziness than others.
During the second trimester, diziness may be caused because your growing uterus puts pressure on blood vessels.
Dizziness may also occur later in your pregnancy if you lie on your back, allowing the weight of the baby to press on your vena cava (a large vein that carries blood from your lower body to your heart).
What remedies exist to prevent dizziness during pregnancy?
There are a number of things you can do to reduce the amount of dizziness you may experience. Here are some helpful suggestions to reduce dizziness during pregnancy:
- Avoid standing for long periods. If you must stand, make sure that you keep your feet moving to help increase circulation
- Get up slowly from either sitting or lying down (This is very important when you are getting out of the bath)
- Eat regularly. Avoid long periods between meals; it is better to snack throughout the day
- Avoid hot baths or showers
- Avoid lying on your back once you reach the middle of your second trimester
- Wear loose, comfortable clothing to avoid restricting circulation
What do I do if I feel faint during pregnancy?
There are a few things you can do to help relieve the feeling that you are going to faint. It is common to faint during pregnancy, so be cautious. Here are some helpful suggestions:
- Avoid getting up quickly from sitting or lying down positions. This is a common reason for dizziness, lightheadedness and fainting.
- If you feel faint, try the following things:
- sit or lie down and lower your head
- take deep breaths
- loosen any tight clothing
- open windows and move towards circulating air
- eat foods rich in iron
When to contact your health care provider because of dizziness during pregnancy:
You should contact your health care provider immediately if your dizziness is accompanied by vaginal bleeding and/or pain in your abdomen. This could be a sign of an ectopic pregnancy, a low-lying placenta, or placental abruption.
You should also contact your health care provider immediately if you have persistent dizziness or dizziness accompanied by blurred vision, headaches, or palpitations; this may be a symptom of severe anemia or some other illness that could have a negative effect on your pregnancy.
Posted by Jennifer at 12:30 PM 1 comments
Labels: General Pregnancy
Week 5
Today marks the start of week 5... and I guess that means I have to start complaining about all my new pregnancy quirks huh? :-)
The day I found out I was pregnant with Arianna started out strange. At 3 o'clock in the morning I woke up with my first asthma attack in years. I remember debating on going to the ER or not as I didn't have a nebulizer anymore. Instead I grabbed a pillow and went to the living room to sleep in the recliner. I slept like crap. That morning, in my sleep deprived haze, I forgot to pack a lunch on my way to work, so I was very hungry throughout the day. My asthma got significantly better as the day went on and I decided to keep my weekly appointment with my personal trainer.
Andrew worked me hard - we were doing upper back and arms that day and toward the end of my 5 set/15 lbs/30 rep arm curls I got dizzy... really dizzy, but I managed to stay standing and finish. I was pretty sure it was due to me not eating that day.
I was totally exhausted when we finished, I got my money's worth! But I knew I wouldn't be up to cooking dinner so I decided to go next door and get us dinners from Boston Market.
While waiting in line I got super dizzy and before I knew it I had passed out - cold. On the floor. The staff was generous, helped me up. Got me water and offered to call an ambulance. I turned down that offer but sat in one of the booths for a few minutes before driving home with, my free, dinner.
I pulled into the driveway the same time my husband was arriving home. He reminded me he was meeting friends for dinner, but in true 'guy fashion' offered to still eat the dinner I got him. I told him about my dizzy spell and that I was just going to lie down for the evening.
We ate dinner. He left. I settled into the bed with my laptop and started surfing the net looking up reasons to be dizzy, mostly for my own amusement. The first thing that came up was being pregnant. I knew my period was late but I was used to erratic periods and was on the birth control patch. In fact I had taken a test 2 days prior and it was negative. But I still had one left in the pack and decided to take it.
Sure enough it came up pregnant.
I freaked. No way could I be pregnant... no freakin' way. I tried calling Shawn, he didn't answer. I called my Mom and cried to her. I was so upset. My dad was there and had been drinking. He flipped out. He kept saying 'you can come home' blah blah blah (not sure where that train of thought came from, we'd been married for 3 years) and eventually over the course of the evening would say something really stupid that caused such a big rift he wouldn't see his granddaughter until she was 6 months old. Finally got a hold of Shawn and told him he needed to come home right now.
I was shaking and crying when he came home and showed him the test. He was so happy (huh?) and excited. He immediately called his family. They were happy - what a contrast to my family. I was devastated - I was going to CA in 2 weeks to participate in a world record skydiving jump... and now I couldn't. I was so sad.
Fast forward 2 years 4 months. Pregnancy #2.
We're actually trying to get pregnant and succeed! I'm happy, he's happy, his family is happy. Mine doesn't know and won't for some time. (oh but I did tell my brother and his girlfriend who I know will keep it quiet)
No major asthma attack. But dizzy? Oh ya...
All. The. Time.
I feel like I'm in a fog, like I don't have control over my body - my hands are shaking alot and I feel like I could fall over even when I'm sitting. I'm not overly concerned but don't know if I should be.
Maybe that means this one is a boy? ;-)
Posted by Jennifer at 12:08 PM 2 comments
Labels: pregnancy 1, pregnancy 2
Thursday, January 10, 2008
Prevention of recurrent preterm delivery by 17 Alpha-Hydroxyprogesterone Caproate
New England Journal of Medicine Abstract
Volume 348:2379-2385
June 12, 2003
Number 24Prevention of Recurrent Preterm Delivery by 17 Alpha-Hydroxyprogesterone Caproate
Paul J. Meis, M.D., Mark Klebanoff, M.D., Elizabeth Thom, Ph.D., Mitchell P. Dombrowski, M.D., Baha Sibai, M.D., Atef H. Moawad, M.D., Catherine Y. Spong, M.D., John C. Hauth, M.D., Menachem Miodovnik, M.D., Michael W. Varner, M.D., Kenneth J. Leveno, M.D., Steve N. Caritis, M.D., Jay D. Iams, M.D., Ronald J. Wapner, M.D., Deborah Conway, M.D., Mary J. O'Sullivan, M.D., Marshall Carpenter, M.D., Brian Mercer, M.D., Susan M. Ramin, M.D., John M. Thorp, M.D., Alan M. Peaceman, M.D., for the National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network
Background:
Women who have had a spontaneous preterm delivery are at greatly increased risk for preterm delivery in subsequent pregnancies. The results of several small trials have suggested that 17 alpha-hydroxyprogesterone caproate (17P) may reduce the risk of preterm delivery.Methods:
We conducted a double-blind, placebo-controlled trial involving pregnant women with a documented history of spontaneous preterm delivery. Women were enrolled at 19 clinical centers at 16 to 20 weeks of gestation and randomly assigned by a central data center, in a 2:1 ratio, to receive either weekly injections of 250 mg of 17P or weekly injections of an inert oil placebo; injections were continued until delivery or to 36 weeks of gestation. The primary outcome was preterm delivery before 37 weeks of gestation. Analysis was performed according to the intention-to-treat principle.Results:
Base-line characteristics of the 310 women in the progesterone group and the 153 women in the placebo group were similar. Treatment with 17P significantly reduced the risk of delivery at less than 37 weeks of gestation (incidence, 36.3 percent in the progesterone group vs. 54.9 percent in the placebo group; relative risk, 0.66 [95 percent confidence interval, 0.54 to 0.81]), delivery at less than 35 weeks of gestation (incidence, 20.6 percent vs. 30.7 percent; relative risk, 0.67 [95 percent confidence interval, 0.48 to 0.93]), and delivery at less than 32 weeks of gestation (11.4 percent vs. 19.6 percent; relative risk, 0.58 [95 percent confidence interval, 0.37 to 0.91]). Infants of women treated with 17P had significantly lower rates of necrotizing enterocolitis, intraventricular hemorrhage, and need for supplemental oxygen.Conclusions:
Weekly injections of 17P resulted in a substantial reduction in the rate of recurrent preterm delivery among women who were at particularly high risk for preterm delivery and reduced the likelihood of several complications in their infants.Preterm delivery — that is, delivery before 37 completed weeks of gestation — is the major determinant of infant mortality in developed countries.1 Preterm delivery is more common in the United States than in many other developed countries and is the factor most responsible for the relatively high infant mortality in this country.1 The rate of preterm delivery in the United States has increased progressively from 9 percent to 12 percent over the past two decades.2 Despite many trials of reduced activity, tocolytic therapy, antibiotic therapy, and other strategies for prevention, no effective and reproducible method of preventing preterm delivery has been demonstrated.3
One treatment that showed promise in small trials was prophylactic treatment with progestational compounds.4,5,6,7 Not all trials reported positive results.8,9 One meta-analysis found no evidence of effectiveness of progestational compounds in the prevention of preterm delivery or the prevention of recurrent miscarriage.10 Another meta-analysis, restricted to trials of 17 alpha-hydroxyprogesterone caproate (17P), a natural metabolite of progesterone, showed, in composite, a significant reduction in the rate of preterm delivery.11 We therefore chose this pharmacologic agent as the active drug for our study.
Women who have had a preterm delivery are at especially high risk for preterm delivery in a subsequent pregnancy.12 We therefore conducted a multicenter trial to test the effectiveness of 17P as compared with placebo in the prevention of recurrent preterm delivery in this group of women.
Posted by Jennifer at 2:46 PM 0 comments
Labels: pPROM, Premature Birth, Preterm Labor
STUDY: Diet influence preterm delivery?
Diet influences preterm delivery?
Issue 23: 14 Nov 2005
Source: American Journal of Obstetrics & Gynecology 2005; 193: 1292-301
Adopting a cholesterol-lowering diet could reduce the risk of preterm delivery in low-risk pregnancies, according to the findings of a new study.
Specialists from centers in Oslo, Norway, randomly assigned 290 women aged 21-38 years to, from 17-20 weeks’ gestation onwards, either continue their usual diet or to adopt a diet with a high intake of fish, low-fat meats and dairy products, oils, whole grains, fruits, vegetables, and legumes.
The women in the dietary intervention group met with a dietician at the start of the study and at weeks 24, 30, and 36 of their pregnancy. The diet (described in detail in the published paper) included limiting the intake of cholesterol to 150 mg/day, reducing saturated fat to 8% of total energy intake, and aiming at a weight gain of 8-14 kg from pre-pregnancy levels.
All of the women in the study were non-smoking, white, with singleton pregnancies, and had no previous pregnancy-related complications. About two-thirds were nulliparous.
Lipids lowered
Writing in the latest issue of the American Journal of Obstetrics & Gynecology, the researchers report that maternal levels of total cholesterol and low-density lipoprotein were significantly lower in the intervention group than in the control group. There were no differences between the two groups in levels of cord and neonatal lipids.
Overall, one of the 141 women in the dietary intervention group had a preterm delivery (defined as a live delivery before 37 completed weeks of gestation), compared with 11 of the 149 women in the control group. This was a statistically significant difference. There were no differences between the groups in the incidence of other pregnancy complications.
The researchers write: “In conclusion, a diet that was reduced in saturated fat and cholesterol, and enriched in a number of micronutrients, modified maternal cholesterol levels, but not cord and neonatal lipids. It was associated with a lower incidence of preterm delivery in low-risk pregnancies and had no adverse effects.”
They say the findings warrant replicating the study in a larger population of pregnant women, involving both low-risk and high-risk pregnancies: “The marked observed effect of this diet on the reduction of preterm delivery in low-risk pregnancies should encourage future larger studies to clarify the role of such a diet in the prevention of preterm birth.”
Posted by Jennifer at 2:09 PM 0 comments
Labels: Premature Birth
STUDY: Prior Miscarriage Raises Risk for Low-Birthweight Infant
Prior Miscarriage Raises Risk for Low-Birthweight Infant
THURSDAY, Dec. 20 (HealthDay News) -- Women who've had a miscarriage or an abortion are much more likely than women who haven't to experience a low-birthweight or premature baby in the future, new research shows.
A team at Virginia Commonwealth University looked at data on more than 45,500 mother-and-child pairs enrolled in the United States Collaborative Perinatal Project.
About 40 percent of the mothers had one or two children, and almost two-thirds of the mothers were between ages 20-29. The researchers found that rates of low-birthweight (under 2,500 grams or 5.5 pounds) and premature babies (less than 37 weeks gestation) were highest among women who were black, young or old, poorly educated, and unmarried.
The study also found that women who'd had one, two, or three or more miscarriages or abortions in the past were almost three, five and nine times, respectively, more likely than normal to have an underweight baby.
Women who'd had one miscarriage or abortion were 67 percent more likely to have a premature baby, while women who'd had three or more miscarriages or abortions were more than three times as likely to have a premature baby, compared to women who hadn't had a miscarriage or an abortion.
The study is published in the Journal of Epidemiology and Community Health.
The researchers noted that previous studies have been inconclusive, with some reporting no increased risk and others identifying a significantly increased risk of low-birthweight or premature babies among women who've had a miscarriage or abortion. Despite the conflicting evidence, women and doctors need to be aware of the potential risks, the authors concluded.
-- Robert Preidt
I always have to chuckle at these studies...
"The researchers found that rates of low-birthweight (under 2,500 grams or 5.5 pounds) and premature babies (less than 37 weeks gestation) were highest among women who were black, young or old, poorly educated, and unmarried."
Hmm... so where do I fit? I had a micro-preemie, I'm white, 27 (is that old or young?), am college educated and married... also had extra prenatal care. Where does that put me?
That puts me in the "we don't know why and don't know how to prevent..." category. Just where I longed to be! (that was sarcastic if you didn't catch that)
Posted by Jennifer at 10:51 AM 0 comments
Labels: Premature Birth
Wednesday, January 9, 2008
Causes of preterm birth
Although the cause is often unknown, a variety of factors play a role in preterm birth:• Certain genital tract infections, such as chlamydia, bacterial vaginosis (BV), and trichomoniasis, are associated with preterm delivery.
Substances produced by bacteria can weaken the membranes around the amniotic sac and cause it to rupture early. Even when the membranes remain intact, bacteria can cause preterm labor if they get into the amniotic fluid or sac.
You may have been checked for chlamydia and gonorrhea at your first prenatal visit, and you would have been treated immediately if you'd tested positive for either of these sexually transmitted infections.
If you've had a previous preterm birth, you may also have been screened for bacterial vaginosis. Although some studies show that treating BV in the second and third trimesters reduces the risk of preterm labor in women with a history of preterm birth, other research has found that it makes no difference. So experts don't agree on whether it's worthwhile to test pregnant women who don't have symptoms. (If you have symptoms of bacterial vaginosis, you'll be tested and treated with antibiotics, if needed.)
You probably won't be tested for trichomoniasis unless you have symptoms. Some research suggests that treating women for trichomoniasis during pregnancy actually increases the risk of preterm birth.• Having a problem with the placenta, such as placenta previa or placental abruption.
• Having structural abnormalities of the uterus or cervix, such as a cervix that's shorter than 25 millimeters and that effaces or dilates without contractions (cervical insufficiency).
• Having an excessively large uterus, which is often the case when you're pregnant with multiples or have too much amniotic fluid.
• Certain chronic maternal illnesses may be related to preterm labor, such as diabetes, sickle cell anemia, severe asthma, lupus, inflammatory bowel disease, and chronic active hepatitis. Other conditions to watch for include non-uterine infections, such as a kidney infection or pneumonia; abdominal surgery, such as having your appendix taken out; trauma to the abdomen; and periodontitis (a gum infection that goes into the bone and other tissues that support your teeth).
Preeclampsia
Preeclampsia is a disorder that occurs only during pregnancy and the postpartum period and affects both the mother and the unborn baby. Affecting at least 5-8% of all pregnancies, it is a rapidly progressive condition characterized by high blood pressure and the presence of protein in the urine. Swelling, sudden weight gain, headaches and changes in vision are important symptoms; however, some women with rapidly advancing disease report few symptoms.
Typically, preeclampsia occurs after 20 weeks gestation (in the late 2nd or 3rd trimesters or middle to late pregnancy), though it can occur earlier. Proper prenatal care is essential to diagnose and manage preeclampsia. Preeclampsia, Pregnancy Induced Hypertension (PIH) and toxemia are closely related conditions. HELLP Syndrome and eclampsia are other manifestations of the same syndrome. It is important to note that research shows that more women die from preeclampsia than eclampsia and one is not necessarily more serious than the other.
Preeclampsia and other hypertensive disorders of pregnancy are a leading global cause of maternal and infant illness and death. By conservative estimates, these disorders are responsible for 76,000 deaths each year.
Posted by Jennifer at 4:58 PM 0 comments
Labels: Incompetant Cervix, Infection, Placenta Previa/Abruption, pPROM, Preterm Labor
Week 4
So week 4 is almost finished... and I feel really good. I'm getting pretty constant headaches but they're dull and bearable. I've had some significant dizzy spells the last few days but I expect them as I had a pretty severe 'passing out spell' when I was pregnant with Arianna. I'm only a little tired and my breasts are only a little sore. Honestly, if I didn't have a positive test (ok, so I took a dozen of them) I doubt I would realize I was pregnant!
I'm already making adjustments to my diet - more protein and water throughout the day. I've also added a fish oil capsule to my regular prenatal vitamin and am eating Dannon Activia yogurt during the day to help maintain a healthy balance of the good bacteria in my system. Hopefully this will help my body fight off any infections that could threaten my pregnancy.
My first appointment is still many weeks away and I'll be on pins and needles until I get to see our new miracle on ultrasound and get to talk to my doctor about 'the plan of action' for my pregnancy.
Posted by Jennifer at 2:13 PM 0 comments
Labels: pregnancy 2
Thursday, January 3, 2008
My chart

Hubby and I used fertilityfriend.com to track my cycle. I also used ovulation predictor tests (OPK) and timed intercourse around my most fertile time frame. Then I used pregnancy tests from 8 days past ovulation to test for a positive pregnancy.
I order my a super large batch of ovulation predictor tests and pregnancy tests on eBay, from the Medical Diagnostic Test store
This was our first month trying... I think I should change my name to Myrtle.
Posted by Jennifer at 3:08 PM 0 comments
Labels: pregnancy 2
I'm pregnant!
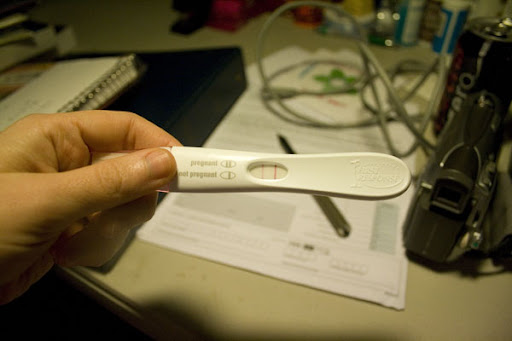
Isn't that a great New Years Day surprise?
Our anniversary is tomorrow and I'm going to surprise my husband with the news!
WOW!
Posted by Jennifer at 9:49 AM 0 comments
Labels: pregnancy 2